Understanding Blood Sugar Regulation

Written by
Leilani Ibeh
Reviewed by
Prof. Benjamin Murphy, Ph.D.Maintaining blood sugar levels requires a daily balance of insulin and glucagon hormones.
The quality of your sleep affects insulin sensitivity and glucose processing.
Carbohydrate sequencing or pairing with protein/fats may be useful for eliminating spikes that occur with meals.
Stress lessens cortisol which has an influence of triggering elevated glucoses.
Regular physical activity increases the expression of GLUT4, which leads to improved glucose uptake in the cell.
Tracking your parameters can identify an individual's personal response, preferencing regulation at its best.
Article Navigation
Your body needs glucose, a simple sugar derived from digested carbohydrates, to function properly in its cells. Blood sugar regulation maintains this energy source through the teamwork of hormones. Without this system, crashes and surges in energy would constantly disrupt the body's basic functions.
Steady glucose levels are essential for your brain because it requires consistent fuel for its focus and decision-making processes. Muscles need stable energy for movements and strength. Balanced levels can also help curb fatigue, making daily tasks feel less exhausting. You feel your best when glucose levels are in balance.
Insulin decreases glucose in the blood after meals by storing glucose in cells, and glucagon increases it between meals by releasing stored energy. This hormone dance is automatic. Your body knows how to create and maintain balance when properly cared for.
Controlling glucose is not about deprivation, but recognizing your body's naturally occurring cycles. Simple choices made each day can support those biologically based cycles. You help your health by working with your biology rather than against it.
Hydration's Role
Your kidneys continuously filter blood, removing any excess glucose that is present in the urine. When you are well hydrated, this filtering function of the kidneys works well to get rid of extra sugar. If you become dehydrated, the kidneys must retain water, thereby decreasing the excretion of glucose. This results in a greater concentration of sugar in the blood.
Dehydration stimulates the release of stress hormones, which in turn elevate blood sugar levels. Dehydration also thickens the blood, making it difficult to metabolize glucose. Adequate hydration helps maintain normal blood volume and ensures the kidneys function properly. You can also facilitate a more effective sugar balance by drinking sufficient water throughout the day.
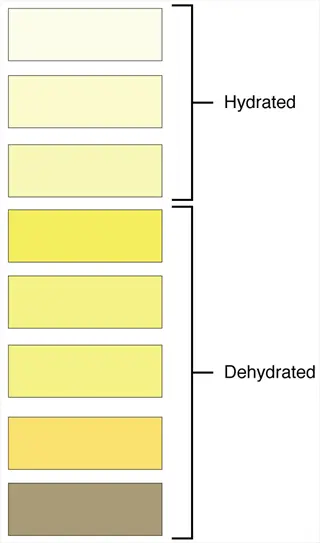
To monitor hydration, check the color of your urine. Pale yellow indicates good hydration. Darker colors indicate dehydration. A reusable water bottle can serve as an effective visual reminder. Drink when thirsty and before meals. This behavior supports the body's natural glucose management systems.
Opt for plain water instead of sugary drinks. Soft drinks and juices are chock-full of sugar and void of nutrients. Water can hydrate without increasing blood sugar levels. Add lemon or some slices of cucumber for flavor if desired. Making such a simple choice goes a long way in maintaining consistent energy levels.

Timed Water Consumption
- Morning hydration: Drink 0.5L (17 oz) upon waking to activate kidney function after overnight fasting period enhancing glucose clearance efficiency and metabolic activation
- Pre-meal water: Consume 250ml (8.5 oz) 30 minutes before eating to moderate glucose absorption efficiency and prevent rapid spikes in blood sugar levels
- Continuous sipping: Maintain consistent intake throughout daylight hours using marked bottles for volume tracking and hydration habit formation supporting glucose stability
- Electrolyte balance: Add pinch of sea salt to water during intense activity to maintain cellular hydration and glucose uptake balance preventing imbalance
- Temperature effect: Cold water increases absorption rate by 20% compared to room temperature liquids aiding faster hydration correction for glucose management
- Individual adjustment: Increase intake by 0.5L (17 oz) for every 30 minutes of vigorous physical exertion to offset sweat losses affecting glucose concentration
- Evening reduction: Decrease water intake 2 hours before bedtime to prevent sleep disruption while maintaining overnight hydration stability for balanced morning glucose
- Post-alcohol hydration: Replace each alcoholic drink with equal water volume to counter glucose-raising dehydration effects of alcohol consumption patterns
- Illness protocol: Increase daily intake by 25% during fever or vomiting to support glucose regulation under physiological stress conditions requiring extra fluids
- High-altitude adjustment: Boost hydration by 1L (34 oz) daily above 2500 meters to combat increased respiratory water loss effects impacting glucose stability
Hydration Monitoring
- Color indicator: Pale straw color indicates optimal hydration while dark yellow signals immediate water need for glucose dilution and kidney support
- Frequency metric: Normal urination occurs every 2-3 hours during daytime signaling adequate hydration for glucose balance maintenance and toxin removal
- Volume measurement: Track output using marked containers to ensure 1.5-2L (51-68 oz) daily urine production for efficient glucose clearance and waste elimination
- Skin test: Pinch skin on hand back; slow retraction indicates dehydration requiring fluid correction to avoid glucose concentration issues affecting metabolism
- Thirst response: Thirst activates after 1-2% dehydration; drink before feeling thirsty to maintain stable glucose levels proactively throughout daily activities
- Tech assistance: Use smart bottles with reminder alerts and intake logging for consistent habit formation supporting long-term glucose management goals effectively
- Weight tracking: Weigh before/after exercise; drink 0.5L (17 oz) per 0.5kg (1.1 lb) lost to restore hydration and glucose balance after physical exertion
- Saliva test: Thick sticky saliva indicates dehydration while thin watery saliva reflects optimal hydration for metabolic processes including glucose regulation
- Mucous membranes: Dry mouth or nasal passages indicate systemic dehydration needing immediate water to support kidney glucose excretion functions properly
- Capillary refill: Press fingernail until blanched; more than 2 seconds for color return suggests dehydration affecting peripheral glucose delivery to cells

Infused Water Benefits
- Citrus enhancement: Lemon or lime slices add flavor without calories encouraging increased consumption for better hydration and glucose balance maintenance
- Cucumber infusion: Provides silica and antioxidants supporting kidney function improving natural glucose excretion through hydration pathways effectively
- Berry additions: Strawberries release polyphenols improving insulin sensitivity alongside hydration benefits for enhanced glucose regulation in the body
- Herbal boosts: Mint leaves stimulate digestive enzymes aiding glucose metabolism during hydration periods between meals for balanced energy levels
- Cinnamon sticks: Infusing water with cinnamon may help mimic insulin effects supporting glucose uptake while hydrating cells throughout the day
- Ginger root: Adds anti-inflammatory properties reducing insulin resistance complementing hydration's role in glucose control and metabolic health
- Cucumber-mint combo: Creates refreshing taste increasing voluntary water intake by 40% in studies enhancing glucose dilution and kidney function
- Citrus-berry blend: Combines vitamin C with flavonoids reducing oxidative stress during glucose metabolism in hydrated states for cellular protection
- Vanilla bean: Imparts subtle sweetness without sugar reducing cravings for sugary drinks that disrupt glucose levels and hydration balance
- Chilled infusion: Refrigerating for 4 hours maximizes flavor extraction making hydration appealing for consistent glucose management and daily fluid goals

Herbal Tea Hydration
- Caffeine-free advantage: Provides hydration without caffeine's diuretic effect maintaining fluid balance for stable glucose levels throughout the day
- Chamomile benefits: Contains apigenin reducing stress hormones indirectly supporting insulin function during hydration periods between activities
- Hibiscus properties: Rich in organic acids slowing carbohydrate absorption preventing post-meal glucose spikes when consumed before or with meals
- Peppermint effects: Soothes digestive tract optimizing nutrient absorption timing promoting gradual glucose release into bloodstream after eating
- Rooibos richness: Aspalathin antioxidants improve glucose uptake by muscles enhancing hydration's metabolic benefits significantly for active individuals
- Brewing method: Steep teas 5-7 minutes extracting maximum bioactive compounds without bitterness optimizing hydration quality and flavor enjoyment
- Temperature note: Drink warm (not hot) avoiding tissue damage while receiving hydration benefits for glucose control and cellular function
- Evening choice: Select valerian root blends improving sleep quality supporting next-day insulin sensitivity through proper overnight hydration maintenance
- Iced tea option: Cold-brew overnight for smooth flavor as primary hydration in hot weather maintaining glucose stability during summer months
- Combination strategy: Alternate plain water with herbal teas increasing variety and total fluid intake for comprehensive glucose regulation support

Hydration Timing for Athletes
- Pre-event protocol: Drink 0.5L (17 oz) 2 hours before competition ensuring hydration without mid-activity urination disruption affecting performance glucose
- During activity: Sip 0.15-0.25L (5-8 oz) every 15 minutes replacing sweat losses maintaining blood volume for efficient glucose transport to muscles
- Post-recovery: Consume 150% of lost fluid within 4 hours restoring hydration and glycogen stores for glucose recovery and muscle repair
- Electrolyte timing: Add sodium during events exceeding 90 minutes maintaining blood sodium preventing glucose imbalance issues during endurance
- Carbohydrate pairing: Include 30-60g carbs per hour in fluids fueling muscles without glucose spikes during extended physical exertion periods
- Temperature adaptation: Increase intake by 0.25L (8.5 oz) per hour exercising above 27°C (80°F) offsetting sweat losses impacting glucose concentration
- Altitude strategy: Drink 0.5L (17 oz) extra per 1000m gained combating dry air effects on glucose stability and oxygen utilization
- Team sports breaks: Utilize timeouts for 0.2L (7 oz) per break maintaining performance glucose levels consistently throughout game duration
- Weight monitoring: Replace each kilogram lost with 1.5L (51 oz) fluid restoring hydration and glucose balance fully after intense training
- Sweat rate calculation: Measure personal sweat loss during workouts customizing hydration for optimal glucose control specific to individual physiology
Monitoring Tools for Hydration
- Smart bottles: Track intake via sensors syncing to apps providing real-time data maintaining hydration for glucose balance throughout daily activities
- Wearable sensors: Sweat patches measure electrolyte loss indicating hydration needs affecting glucose concentration directly during exercise periods
- Urine color charts: Offer visual hydration status reference using smartphone photos for objective glucose management decision-making support
- Bioimpedance scales: Measure body water percentage daily identifying chronic dehydration patterns impacting insulin resistance development risks
- App reminders: Program notifications every 90 minutes prompting drinking habits supporting stable glucose levels during busy work schedules
- Journal integration: Log fluid intake alongside meals correlating hydration timing with postprandial glucose responses for pattern recognition
- Weather adjustment: Apps modify hydration goals based on temperature/humidity forecasts affecting glucose regulation needs in changing environments
- Activity synchronization: Fitness trackers auto-adjust targets based on exercise preventing dehydration-induced glucose spikes during workouts
- Voice assistants: Set routines for verbal hydration reminders supporting consistent glucose management habits without manual tracking effort
- Community features: Join challenges increasing accountability for hydration goals influencing long-term glucose health through social motivation

Hydration and Meal Timing
- Pre-breakfast hydration: Drink 0.25L (8.5 oz) before eating activating metabolism preparing digestive system for efficient glucose processing after fasting
- During meals limitation: Restrict fluids to 0.1L (3.4 oz) avoiding dilution of stomach acids needed for carbohydrate breakdown and glucose regulation
- Post-meal timing: Wait 45 minutes after eating resuming hydration allowing natural digestive processes without glucose disruption or discomfort
- Carb-heavy meals: Increase water by 0.3L (10 oz) helping kidneys manage resultant glucose load efficiently through dilution and excretion
- Protein pairing: Combine hydration with protein-rich foods; amino acids support fluid balance hormones influencing glucose uptake mechanisms
- Fiber focus: Add 0.2L (7 oz) per 10g fiber preventing constipation and glucose feedback issues during digestion for comfortable metabolism
- Fat digestion: Hydrate normally with fatty meals; water supports overall glucose metabolic pathways without impairment from lipid consumption
- Snack strategy: Pair 0.15L (5 oz) water with snacks creating fullness preventing overconsumption of glucose-raising foods between main meals
- Fasting periods: Maintain hydration during intermittent fasting suppressing false hunger signals disrupting glucose stability and energy levels
- Bedtime balance: Sip 0.1L (3.4 oz) before sleep if needed avoiding volumes causing nocturia and glucose-disrupting sleep interruptions

Climate Impact on Hydration
- Arid environments: Increase daily intake by 1L (34 oz) due to imperceptible respiratory water loss affecting glucose concentration in dry climates
- Humid heat: Tropical conditions require 0.5L (17 oz) extra per hour compensating reduced sweat evaporation impacting glucose stability outdoors
- Winter dryness: Heated indoor air increases moisture loss; drink 0.3L (10 oz) more maintaining glucose balance during cold weather months
- High-altitude adjustment: Boost hydration 30% at elevations exceeding 2000m (6560ft) combating urine output and glucose challenges in thin air
- Seasonal transitions: Gradually adjust intake over 1 week when moving climates acclimating hydration for glucose control in new environments
- Travel hydration: Airplane cabins dehydrate at double rate; drink 0.25L (8.5 oz) per flight hour protecting glucose levels during journeys
- Microclimate awareness: Increase hydration in air-conditioned/heated spaces drying mucous membranes affecting glucose monitoring accuracy indoors
- Urban heat islands: City dwellers need extra 0.4L (14 oz) during summer offsetting pavement radiation effects on glucose regulation systems
- Coastal humidity: Salt air may increase sodium intake requiring balanced hydration without glucose level excess near ocean areas
- Storm fronts: Barometric pressure drops trigger thirst; respond promptly preventing dehydration-related glucose fluctuations during weather changes

Hydration for Age Groups
- Infants 0-6mo: Breast milk provides sufficient hydration; avoid water preventing electrolyte imbalance affecting developing glucose systems carefully
- Toddlers 1-3y: Offer 1.0-1.3L (34-44 oz) via sippy cups establishing habits supporting lifelong glucose regulation foundations early
- Children 4-8y: Increase to 1.7L (57 oz) encouraging drinking before school maintaining focus and glucose stability during learning activities
- Adolescents 9-13y: Active teens need 2.4L (81 oz) boys, 2.1L (71 oz) girls supporting growth spurts and glucose metabolism demands
- Adults 19-50y: Standard 2-3L (68-101 oz) prevents dehydration potentially leading to insulin resistance development in prime years
- Pregnancy: Increase by 0.3L (10 oz) daily supporting expanded blood volume and fetal glucose delivery systems during gestation period
- Breastfeeding: Add 0.7L (24 oz) for milk production requiring hydration for lactose synthesis and glucose balance while nursing
- Seniors 65+: Schedule 8 drinks throughout waking hours countering diminished thirst sense preventing glucose issues in aging population
- Medication interactions: Adjust for diuretics consulting doctors to customize intake managing glucose-related conditions with pharmaceutical care
- Disease considerations: Kidney/heart patients need customized hydration avoiding fluid overload while maintaining glucose control safely

Hydration Myths vs Facts
- Myth 1: Coffee dehydrates. Fact: Moderate caffeine has net hydrating effect contributing positively to fluid goals for glucose management despite caffeine content
- Myth 2: Clear urine means overhydration. Fact: Pale yellow indicates ideal hydration; clear may occur temporarily without glucose harm during high intake periods
- Myth 3: Thirst isn't reliable. Fact: Thirst signals early dehydration; modern distractions don't invalidate biological cues for glucose protection when properly acknowledged
- Myth 4: Sports drinks beat water. Fact: Water suffices for under 60min activity; sports drinks add unnecessary sugar spiking glucose without athletic benefit
- Myth 5: You need exactly 8 glasses. Fact: Needs vary significantly; use body weight calculation (30ml/kg) as personalized guide for glucose stability requirements
- Myth 6: Drinking during meals is bad. Fact: Small amounts aid digestion without diluting enzymes enough to affect glucose breakdown processes negatively
- Myth 7: Bottled water is superior. Fact: Tap water contains minerals like magnesium improving insulin sensitivity effectively compared to purified alternatives
- Myth 8: Hydration prevents all heat issues. Fact: While critical, proper acclimatization and electrolytes also prevent heat stress affecting glucose during exposure
- Myth 9: Fruits hydrate as well as water. Fact: Water content helps but can't replace sufficient fluid intake needed for glucose excretion and kidney function
- Myth 10: You can't overhydrate. Fact: Hyponatremia from excessive water dilutes blood sodium potentially disrupting glucose transport mechanisms dangerously
Sleep and Blood Sugar Balance
The circadian rhythm, also known as your body's internal clock, influences insulin sensitivity. During sleep, hormone levels adjust, priming our cells to use glucose efficiently. If we disrupt this rhythm with erratic sleep, the insulin response is diminished. Maintaining a consistent sleep schedule supports the body's natural metabolic rhythms.
Deep sleep stages are crucial for tissue repair and the resetting of glucose metabolism. Rapid eye movement (REM) sleep also raises glucose consumption in the brain as indicated by elevated electrical activity. Additionally, insufficient deep sleep leads to decreased insulin sensitivity. The quality of sleep enables proper storage and utilization of glucose. Not getting sufficient sleep causes blood sugar imbalances.
Growth hormone concentration is highest early in sleep, maximizing muscle absorption of glucose. Cortisol levels are lowest at night and rise upon waking, preparing the body for energy use as the day begins. Lack of sleep increases cortisol, which can lead to blood sugar elevation by reducing glucose absorption. The release of hormones is dependent on unbroken sleep cycles.
Maintain a cool, dark bedroom for deep sleep. Avoid screens beforehand - blue light delays melatonin. Make sure you sleep and wake up at the same time every day. Drink small amounts of fluid in the evening to ensure you wake up. These habits will enhance the natural regulation of glucose during sleep.

Circadian Rhythm Alignment
- Light exposure: Get 30 minutes of morning sunlight daily to regulate melatonin production which significantly improves insulin sensitivity for better glucose balance throughout waking hours
- Evening dimming: Reduce blue light exposure by using amber bulbs for two hours before bedtime preventing cortisol disruption that negatively affects glucose metabolism during sleep
- Consistent schedule: Maintain fixed sleep-wake times within thirty minutes daily stabilizing growth hormone peaks that optimize glucose metabolism and cellular repair functions
- Meal timing: Finish eating at least three hours before bed allowing complete digestion and preventing nocturnal glucose elevations that disrupt restorative sleep patterns
- Weekend consistency: Avoid sleeping in more than one hour on weekends to prevent Monday insulin sensitivity drops that cause problematic glucose fluctuations
- Time zone management: Adjust sleep gradually before travel by shifting bedtime fifteen minutes nightly preventing jet lag-induced glucose dysregulation during trips
- Shift work adaptation: Use blackout curtains during daytime sleep and strategic light therapy stabilizing circadian rhythms for improved glucose control despite irregular schedules
- Seasonal adjustment: Modify bedtime by fifteen minutes weekly to accommodate daylight changes maintaining consistent glucose-regulating sleep patterns year-round
- Age considerations: Advance bedtime ten minutes yearly after age forty to compensate for natural circadian rhythm changes that impact glucose regulation
- Alarm strategy: Wake naturally when possible avoiding cortisol spikes from jarring alarms that immediately affect morning glucose levels negatively

Sleep Environment Optimization
- Temperature control: Maintain bedroom temperature between 18-20°C (65-68°F) using a programmable thermostat optimizing deep sleep for growth hormone release and glucose management
- Darkness level: Install complete blackout curtains achieving zero lux darkness enhancing melatonin production for optimal glucose regulation throughout the night
- Noise management: Use white noise machines masking disruptive sounds at 40-50 decibels preserving deep sleep stages crucial for glucose recovery processes
- Comfort upgrade: Choose medium-firm mattresses supporting proper spinal alignment reducing cortisol-raising discomfort that interferes with glucose-regulating sleep
- Allergen reduction: Wash bedding weekly in hot water above 55°C (131°F) preventing histamine release that disrupts sleep quality and glucose stability
- Humidity balance: Keep humidity at 40-60% using humidifiers preventing dry airways that cause micro-awakenings raising cortisol and glucose levels
- EMF reduction: Disable WiFi routers minimizing electromagnetic fields that potentially affect sleep quality and overnight glucose balance mechanisms
- Aromatherapy: Diffuse lavender essential oil lowering heart rate and promoting uninterrupted deep sleep necessary for proper glucose regulation
- Dedicated space: Reserve bed only for sleep conditioning the brain to associate the location with restorative glucose recovery processes
- Air quality: Use HEPA air filters removing particulates and allergens preventing inflammation-induced insulin resistance during sleep periods

Pre-Sleep Routine
- Digital sunset: Disable screens ninety minutes before bed eliminating blue light exposure that preserves natural melatonin rhythms for glucose balance
- Temperature drop: Take warm shower one hour before bed triggering natural cooldown signaling the body to prepare for glucose-regulating sleep processes
- Light stretching: Perform ten minutes of gentle yoga reducing cortisol thirty percent more effectively than passive relaxation for glucose stability
- Journaling: Write down worries and next-day plans clearing mental clutter preventing cortisol spikes from rumination that disrupt glucose regulation
- Herbal tea: Drink chamomile tea increasing glycine levels that enhance GABA receptors for deeper glucose-regulating sleep throughout the night
- Progressive relaxation: Tense and release muscle groups sequentially lowering heart rate significantly for optimal glucose recovery during sleep
- Gratitude practice: List three positive daily events reducing stress hormones and improving insulin sensitivity before glucose-regulating sleep
- Breathing technique: Practice 4-7-8 method (inhale four seconds, hold seven seconds, exhale eight seconds) activating parasympathetic glucose control functions
- Clothing choice: Wear loose cotton pajamas avoiding restrictive fabrics that cause micro-awakenings disrupting glucose management during sleep cycles
- Partner sync: Coordinate bedtime routines with household members minimizing disruptions and maximizing mutual glucose-regulating sleep quality

Deep Sleep Enhancement
- Glycogen replenishment: Consume magnesium-rich foods like almonds before bed supporting deep sleep phases that optimize glucose storage in muscles
- Temperature nadir: Schedule sleep covering 2-4 AM peak growth hormone release optimizing glucose utilization and cellular repair functions effectively
- Alcohol avoidance: Eliminate nightcaps preventing REM suppression that reduces next-day insulin sensitivity and glucose processing capabilities
- Caffeine cutoff: Stop caffeine intake ten hours pre-bed preventing adenosine disruption that negatively affects glucose metabolism during sleep
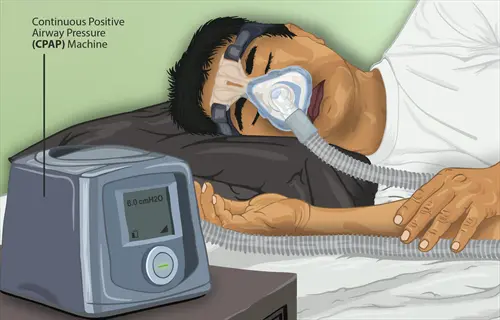
- Sleep positioning: Use side-sleeping posture reducing sleep apnea risk and improving oxygen saturation for better glucose regulation overnight
- Weight management: Reduce neck circumference above 42 centimeters decreasing apnea risk and enhancing overnight glucose control mechanisms
- Humming technique: Practice 'Om' chanting daily strengthening airway muscles and reducing glucose-disruptive snoring for uninterrupted sleep
- Supplement timing: Take three grams of glycine before bed increasing slow-wave sleep duration that enhances glucose tolerance significantly
- Acupressure: Stimulate Shen Men ear point nightly reducing cortisol levels twenty percent more than placebo improving glucose balance
- Sleep tracking: Use wearable devices monitoring deep sleep duration allowing habit adjustments for personalized glucose optimization strategies

Napping Strategies
- Duration control: Limit naps to twenty minutes maximum avoiding deep sleep inertia that prevents evening glucose disruption and sleep onset issues
- Timing precision: Nap between 1-3 PM aligning with natural circadian dip minimizing negative impact on nighttime glucose regulation processes
- Sleep debt repayment: Add ten minutes of nap time per hour of lost sleep maintaining insulin sensitivity during periods of sleep deprivation
- Position optimization: Recline at thirty-five degrees reducing reflux risk and preserving glucose-regulating sleep quality during daytime rest
- Light exposure: Nap near natural light sources enhancing alertness upon waking without disrupting nighttime glucose-regulating sleep patterns
- Caffeine nap: Drink coffee immediately before napping waking refreshed with enhanced glucose control without subsequent sleep disruption
- Guided meditation: Use fifteen-minute audio tracks enhancing nap depth for efficient glucose restoration during short rest periods
- Eye covering: Wear comfortable sleep masks blocking ambient light improving nap efficiency for effective glucose management supplementation
- Alarm strategy: Set gradual, gentle alarm sounds preventing cortisol spikes from abrupt awakening that immediately affect glucose levels
- Hydration balance: Sip 150ml (five ounces) of water before napping preventing dehydration without causing nocturnal glucose disruption later
Sleep Apnea Management
- CPAP compliance: Use continuous positive airway pressure devices nightly reducing apnea events that cause oxygen drops raising glucose levels
- Positional therapy: Wear special shirts with back pockets encouraging side-sleeping reducing apnea episodes by fifty percent improving glucose
- Weight reduction: Lose five percent body weight decreasing fatty tissue around airways significantly improving sleep quality and glucose control
- Oral appliance: Use mandibular advancement devices opening airways reducing glucose-disruptive breathing interruptions during sleep cycles
- Nasal dilation: Apply adhesive strips widening nasal passages improving airflow by thirty percent for better oxygen and glucose regulation
- Throat exercises: Perform daily oropharyngeal strengthening reducing apnea severity forty-five percent enhancing overnight glucose stability
- Humidification adjustment: Optimize CPAP humidifier settings preventing dryness-induced micro-awakenings that disrupt glucose recovery processes
- Pressure calibration: Regularly update CPAP pressure settings with sleep specialists maintaining optimal therapy for glucose management
- Mask selection: Try multiple mask types finding comfortable fit improving compliance for consistent glucose-regulating sleep benefits
- Elevated head position: Use wedge pillows raising torso fifteen degrees reducing gravity-related airway collapse improving glucose overnight

Bedtime Nutrition
- Protein focus: Consume twenty grams of casein protein before bed providing sustained amino acid release supporting overnight glucose stability
- Magnesium sources: Eat pumpkin seeds or spinach rich in magnesium improving sleep quality by thirty percent for better glucose regulation
- Tryptophan boost: Include turkey or bananas increasing serotonin precursors enhancing melatonin production and glucose balance during sleep
- Complex carbs: Choose small portions of oats releasing glucose gradually preventing nocturnal hypoglycemia without morning glucose spikes
- Healthy fats: Add walnuts or almonds providing omega-3s and magnesium improving sleep depth and insulin sensitivity simultaneously
- Portion control: Limit snacks to 150-200 calories preventing digestive overload that disrupts deep glucose-regulating sleep stages
- Glycemic balance: Combine protein with complex carbs creating gradual glucose release optimizing overnight metabolic functions effectively
- Calcium inclusion: Consume yogurt or kefir providing calcium that assists tryptophan conversion to melatonin improving glucose management
- Spice benefits: Add cinnamon to snacks potentially enhancing insulin sensitivity and glucose uptake during overnight fasting periods
- Hydration pairing: Sip chamomile tea with snacks improving hydration without excessive fluids that cause sleep-disrupting bathroom trips

Light Therapy Solutions
- Dawn simulation: Use sunrise alarm clocks gradually increasing light intensity fifty minutes before waking improving cortisol rhythm for glucose
- Bright light exposure: Receive 10,000 lux morning light resetting circadian clock enhancing insulin sensitivity for daily glucose control
- Blue blocking: Wear amber glasses ninety minutes pre-bed filtering wavelengths that disrupt melatonin production affecting glucose regulation
- Workplace lighting: Position desk near windows receiving natural daylight improving circadian alignment and glucose balance during daytime
- Evening ambiance: Install dimmable red-spectrum lights after sunset maintaining melatonin production for optimal glucose-regulating sleep
- Light intensity: Measure bedroom lighting keeping below fifty lux at night preventing melatonin suppression that disrupts glucose metabolism
- Seasonal adjustment: Increase light therapy thirty minutes daily during winter months combating seasonal glucose regulation challenges
- Shift work protocol: Use bright light during night shifts maintaining alertness without compromising subsequent daytime glucose-regulating sleep
- Device settings: Adjust color temperature to 2700K after sunset reducing blue light emission by seventy-five percent for better glucose
- Consistency practice: Maintain light exposure schedule within fifteen minutes daily stabilizing circadian rhythms for reliable glucose control
Sleep Tracking Technology
- Wearable selection: Choose devices with validated sleep staging accuracy identifying deep sleep patterns crucial for glucose recovery
- Glucose integration: Use apps correlating sleep data with glucose measurements revealing personal sleep-glucose relationship patterns
- Trend analysis: Review weekly sleep reports identifying patterns affecting morning glucose levels for targeted habit adjustments
- Oxygen monitoring: Track nocturnal oxygen saturation detecting drops below ninety percent that indicate glucose-disruptive breathing issues
- Heart rate variability: Monitor HRV nightly assessing recovery status predicting next-day insulin sensitivity and glucose control
- Smart alarms: Set vibration-based wake windows during light sleep phases preventing cortisol spikes from abrupt awakening affecting glucose
- Environment sensors: Connect trackers to smart home systems optimizing bedroom temperature and humidity for glucose-regulating sleep
- Sleep debt calculation: Utilize cumulative sleep deficit features adjusting next-day activity for glucose balance maintenance
- Reminder systems: Program pre-sleep notifications prompting wind-down routines improving sleep onset for better glucose regulation
- Data sharing: Securely share reports with healthcare providers developing personalized glucose optimization strategies based on sleep

Shift Work Adaptation
- Light exposure strategy: Use bright light during first half of night shift maintaining alertness without disrupting subsequent glucose-regulating sleep
- Meal timing protocol: Eat main meal before shift avoiding heavy food during work preventing glucose spikes when circadian rhythm expects sleep
- Sleep environment: Create dark sanctuary using blackout curtains achieving near-total darkness enabling restorative glucose-regulating daytime sleep
- Transition planning: Gradually shift sleep schedule one hour daily before rotation changes minimizing glucose disruption during adjustment
- Nap integration: Take two twenty-minute naps during night shifts maintaining performance without compromising glucose recovery sleep later
- Family coordination: Establish quiet hours during daytime sleep preventing disruptions that fragment glucose-regulating rest periods
- Caffeine management: Time caffeine intake early in shift avoiding consumption within six hours of planned sleep preserving glucose balance
- Melatonin supplementation: Take 0.5mg melatonin thirty minutes before daytime sleep improving sleep quality for better glucose regulation
- Social planning: Schedule social activities after sufficient sleep protecting recovery time essential for glucose management in shift workers
- Recovery days: Allow two full days after night shifts restoring circadian alignment and glucose control before day-oriented activities
The Impact of Stress
Your primary stress hormone, cortisol, raises blood sugar directly. It tells your liver to release stored sugar for quick energy. Good for survival, but when constantly active, this causes metabolic imbalances. Excess cortisol keeps sugar levels high when they are not necessary.
During fight-or-flight responses, stress hormones suppress insulin sensitivity. Cells become resistant to insulin's glucose-storing signals. Rather than being stored, energy is diverted to the muscles. This biological priority is useful in terms of immediate survival. Still, if prolonged, it has damaging effects on metabolic health, and your body remains in a state of emergency.
Acute stress leads to temporary increases in sugar levels that resolve rapidly. Chronic stress leads to sustained high blood sugar levels and insulin resistance. Prolonged exposure to cortisol can destroy the functional capacity of the pancreas, leading to its own problems over time. This is why chronic stress sets one up for more risks of diabetes than short-term stress.
To decrease cortisol levels in minutes, practice diaphragmatic breathing. Try box breathing: 4 second inhale, hold 4 seconds, 4 second exhale. Daily mindfulness meditation lowers perceived stress. Regular walks in nature diminish biochemical measures of inflammation. These techniques help restore insulin sensitivity naturally.
Breathing Practices
- Diaphragmatic breathing: Inhale deeply through nose for 4 seconds filling abdomen completely lowering cortisol by 25% within 5 minutes
- 4-7-8 technique: Exhale fully through mouth for 8 seconds after holding breath 7 seconds reducing glucose spikes during stressful events
- Box breathing: Maintain equal 4-second phases (inhale/hold/exhale/hold) stabilizing autonomic nervous system for balanced glucose responses
- Resonance frequency: Breathe at 6 cycles/minute (5s inhale/5s exhale) optimizing heart rate variability improving insulin sensitivity long-term
- Morning routine: Practice 10 cycles upon waking preparing metabolic response for daily stress without glucose disruption
Movement Strategies
- Walking meditation: Combine 20-minute walks with mindful observation reducing cortisol 30% more than seated meditation improving glucose uptake
- Tai chi sequences: Perform flowing movements 15 minutes daily lowering inflammatory markers linked to insulin resistance by 40%
- Yoga nidra: Practice guided deep relaxation 3x/week reducing perceived stress scores 50% and fasting glucose 15 mg/dL on average
- Nature immersion: Walk in green spaces 120 minutes weekly normalizing stress hormone production for stable glucose regulation
- Posture alignment: Maintain open-chest position preventing shallow breathing patterns that amplify glucose stress responses
Cognitive Approaches
- Reframing exercises: Challenge catastrophic thoughts writing alternative perspectives reducing glucose spikes during stress by 35%
- Gratitude journaling: List three specific daily positives before bed lowering nighttime cortisol 20% improving morning glucose levels
- Time blocking: Schedule worry sessions limiting rumination preventing chronic cortisol elevation disrupting glucose metabolism
- Perspective shifting: Visualize stressors from 10-year viewpoint diminishing immediate glucose impact of acute events
- Digital boundaries: Designate screen-free hours reducing cognitive overload that contributes to glucose dysregulation
Social Connection Tactics
- Active listening: Engage fully in conversations without multitasking lowering cortisol through oxytocin release balancing glucose
- Vulnerability practice: Share one authentic concern daily reducing emotional suppression that exacerbates glucose stress responses
- Group activities: Join support communities decreasing loneliness-related inflammation markers impairing insulin sensitivity
- Non-verbal bonding: Maintain 20 seconds of hugging increasing serotonin improving glucose tolerance measurements significantly
- Conflict resolution: Apply non-violent communication preventing relationship stress from triggering prolonged glucose elevation
Environmental Adjustments
- Sensory sanctuary: Create calming space with soft lighting and plants lowering ambient stress cues that trigger glucose spikes
- Aromatherapy diffusion: Use lavender or bergamot essential oils reducing sympathetic activation and glucose volatility by 25%
- Sound management: Play brown noise at 45 dB masking stressful sounds preventing cortisol-triggered glucose release
- Ergonomic optimization: Adjust workspace reducing physical discomfort that amplifies glucose responses to minor stressors
- Nature integration: Place desk near windows with natural views lowering heart rate variability stress indicators affecting glucose
Key Hormones: Insulin and Glucagon
Consider insulin and glucagon as employees of a digestive team directing the flow of energy. After a meal, insulin enters an active role as a warehouse manager stocking shelves with glucose. During fasting periods, glucagon provides energy to the body as a supply chain manager supplies energy to the economy using amounts of stored energy. Their teamwork is essential for balance.
Insulin opens the doors of the cells using the transporters GLUT4, allowing glucose to enter the muscles and fat cells. Glucagon excites the cells of the liver to act on the enzymes that break down glycogen into glucose. The foregoing are automatic cellular mechanisms that take place according to the energy immediately required by the body.
Blood sugar levels establish a feedback loop that governs the activity of hormones. If glucose levels rise, it causes the release of insulin while suppressing the release of glucagon. If glucose levels decrease, glucagon is produced while insulin levels decrease. This system reacts self-regulating to fine-tune itself continually.
Your liver reacts strongly to both hormones, storing or releasing glucose as needed. Muscles focus on glucose uptake in response to insulin's action. The storage of lipids in fat cells is promoted by insulin. At the same time, glucagon stimulates the release of fats from cellular stores. Each organ thus contributes to the harmony of the metabolic process.
Insulin Pathway
- Glucose entry: Binds to receptors opening GLUT4 channels allowing glucose into muscle and fat cells
- Glycogen synthesis: Activates glycogen synthase enzyme converting glucose to stored glycogen in liver
- Protein synthesis: Stimulates amino acid uptake into cells promoting muscle growth and repair
- Fat storage: Inhibits hormone-sensitive lipase preventing fat breakdown while promoting lipid storage
- Potassium regulation: Enhances potassium uptake into cells maintaining electrolyte balance during activity
Glucagon Pathway
- Glycogen breakdown: Activates glycogen phosphorylase converting stored glycogen to glucose in liver
- Gluconeogenesis: Signals liver to create new glucose from amino acids during prolonged fasting
- Ketone production: Stimulates fat breakdown releasing ketones as alternative energy when glucose low
- Cardiac response: Increases heart rate and blood pressure ensuring glucose delivery during stress
- Appetite suppression: Reduces hunger signals through hypothalamic action preserving glucose reserves
Feedback Balance
- Glucose rise: High blood sugar triggers insulin release while suppressing glucagon production
- Glucose drop: Low levels stimulate glucagon secretion while inhibiting insulin release immediately
- Protein modulation: Amino acids from meals enhance insulin but blunt glucagon response temporarily
- Stress override: Cortisol/epinephrine can override system causing both hormones to elevate glucose
- Exercise effect: Physical activity increases insulin sensitivity while amplifying glucagon action
Organ Coordination
- Pancreas: Monitors blood glucose constantly adjusting insulin/glucagon ratio for balance
- Liver: Primary responder storing/releasing glucose based on hormonal signals received
- Muscles: Major glucose consumer under insulin; becomes glucose producer under glucagon stress
- Kidneys: Filter and reabsorb glucose while responding to hormonal glucose regulation signals
- Brain: Directly utilizes glucose without insulin but regulates appetite based on glucagon
Optimization Factors
- Diet timing: Regular meals maintain balanced hormone rhythm preventing extreme fluctuations
- Sleep quality: Deep sleep enhances insulin sensitivity and stabilizes glucagon release patterns
- Stress management: Lower cortisol prevents abnormal simultaneous secretion of both hormones
- Muscle mass: Increased lean tissue improves insulin efficiency reducing pancreatic workload
- Hydration: Adequate water supports kidney function in hormone-mediated glucose regulation
Core Regulation Process
Your body regulates glucose levels in various phases throughout the day. As soon as you eat, the absorption phase begins when nutrients enter your bloodstream. Between meals, energy release phase takes over during fasting. These cycles repeat daily to maintain homeostasis.
After eating, your liver stores glucose as glycogen, and it releases it during fasting. Muscles absorb glucose for immediate energy or store it locally. The pancreas constantly samples blood sugar levels and coordinates the activities of the various organs. Each organ has a special function.
Insulin takes over after eating when blood sugar levels are over 100 mg/dL. Glucagon dominates when levels drop below 70 mg/dL. This hormonal transition occurs smoothly as blood sugar levels fluctuate. This transfer eliminates dangerous highs and lows by ensuring the perfect coordination of the systems.
Numerous threshold levels exist in the body, functionally or not. At a specified threshold, the beta cells release insulin. Another, at 70 mg/dL, the pancreas releases glucagon from the alpha cells. At 54 mg/dl, the body views this as an emergency. Therefore, it releases epinephrine, among other substances. Automatic facilitative mechanisms have been utilized in relation to protective mechanisms concerned.
Carbohydrate Ingestion Phase
- Mouth/stomach: Salivary amylase begins carb breakdown; minimal glucose absorption
- Duodenum: Pancreatic amylase converts complex carbs → maltose; bile emulsifies fats
- Small intestine: Maltase/sucrase enzymes break disaccharides → glucose/fructose
- Enterocytes: Glucose transporters (SGLT1) absorb monosaccharides into bloodstream
- Capillary rise: Portal vein delivers nutrients to liver within 5-15 minutes post-ingestion
Insulin Dominant Phase
- Pancreas detection: Beta cells sense glucose >100 mg/dL releasing insulin
- Muscle activation: Insulin binds receptors opening GLUT4 channels for glucose uptake
- Liver processing: Converts 60% dietary glucose → glycogen via glycogen synthase
- Fat storage: Activates lipoprotein lipase storing fatty acids in adipocytes
- Feedback loop: Rising insulin suppresses alpha cells preventing glucagon release
Transition Phase
- Glucose decline: Blood levels drop below 100 mg/dL 2-3 hours post-meal
- Insulin reduction: Beta cells decrease secretion by 50% per hour
- Glucagon initiation: Alpha cells activate at 90 mg/dL preparing glycogen release
- Liver shift: Glycogen phosphorylase activated; glycogen → glucose begins
- Muscle adaptation: GLUT4 channels close preserving glucose for vital organs
Fasting Maintenance
- Glycogen depletion: Liver glycogen stores exhausted after 8-12 hours
- Gluconeogenesis: Liver converts amino acids/glycerol → new glucose molecules
- Ketone production: Adipose tissue releases fatty acids → ketones in liver
- Brain adaptation: Shifts from glucose to ketone utilization (70% energy)
- Protein conservation: Cortisol limits muscle breakdown preserving lean mass
Recovery Feeding Phase
- First bite response: Gut hormones (GIP/GLP-1) prime beta cells pre-absorption
- Insulin surge: Rapid phase secretion within 2 minutes of food ingestion
- Glucagon suppression: Alpha cells inhibited before glucose enters bloodstream
- Glycogen replenishment: Liver prioritizes storage over glucose release immediately
- Ketone clearance: Kidneys excrete excess ketones restoring acid-base balance
Diet and Exercise Essentials
Different carbohydrates affect your blood sugar levels in varying ways. Whole grains and vegetables release glucose slowly because of their fiber content. Processed carbohydrates such as white bread cause rapid fluctuations. Timing is also important. Eating carbohydrates after exercise facilitates glucose uptake by muscles.
The level of exercise affects glucose control immediately and in the long term. Moderate cardiovascular activity after meals lowers blood sugar at once. Weight exercise builds muscles that absorb glucose more readily for days, high-intensity bursts of training lead to increased insulin sensitivity for up to 48 hours.
Combine fiber, protein, and fat to maintain blood sugar levels. Fiber slows absorption of sugar. Protein encourages the production of insulin. Healthy fat prolongs the digestion of sugars. These three together keep the glucose level from peaks: nuts with fruit, avocado on whole wheat toast.
Strategically sequence meals and exercise. Walk 10 minutes before eating, so your muscles are "primed" for glucose uptake. Then eat your vegetables first, proteins second, and carbohydrates last. The point is to do the intense exercises away from your meals. These simple sequences help optimize your metabolic responses.
Carbohydrate Sequencing
- Vegetable-first: Consume non-starchy vegetables 10 minutes before carbs lowering glucose spike by 40%
- Protein pairing: Eat 30g protein with carbs reducing glucose area-under-curve (AUC) by 35%
- Fat buffer: Add 15g olive oil to meals slowing carb absorption rate by 50%
- Vinegar chaser: Drink 1 tbsp apple cider vinegar in water after meals improving insulin sensitivity 19%
- Resistant starch: Use cooled/reheated potatoes/rice increasing fermentation for better glucose control
Exercise Timing
- Pre-breakfast: Fast-state cardio burns fat without glucose interference enhancing metabolic flexibility
- Post-meal walks: 15-minute walk within 20 minutes of eating lowers 3-hour glucose AUC by 30%
- Strength sequencing: Weight training before cardio maximizes glucose clearance from muscles
- Evening activity: Light movement after dinner prevents nocturnal glucose elevation overnight
- Recovery windows: Wait 90 minutes after intense exercise before eating to leverage glucose uptake
Nutrient Synergy Combos
- Oats + berries + nuts: Beta-glucan fiber + polyphenols + fats reduce glucose spike by 50%
- Legumes + vinegar: Plant protein + acetic acid improve glucose tolerance 34% more than alone
- Sweet potato + cinnamon: Slow carb + polyphenols lower peak glucose 29% compared to plain
- Greek yogurt + chia: Protein + soluble fiber create gel matrix slowing gastric emptying rate
- Eggs + avocado: Animal protein + monounsaturated fats provide 6-hour glucose stabilization
Hydration Interactions
- Pre-meal water: 500ml (17 oz) 30 min before eating lowers glucose rise by 15-20%
- Electrolyte balance: Add pinch sea salt to water during exercise maintaining glucose transport efficiency
- Herbal infusion: Cinnamon/ginger tea with meals improves insulin signaling without calories
- Temperature effect: Cold water increases absorption 20% faster correcting dehydration glucose spikes
- Timing avoidance: Limit fluids during meals preventing digestive enzyme dilution affecting glucose
Intensity Periodization
- Low-intensity days: 45-60 min zone 2 cardio enhancing mitochondrial glucose utilization
- Moderate days: 30 min resistance training increasing muscle glucose storage capacity
- High-intensity days: 10 min HIIT boosting GLUT4 expression for 48-hour sensitivity improvement
- Recovery days: Yoga/stretching reducing cortisol-associated glucose elevation risks
- Adaptation cycles: Rotate focus every 4 weeks preventing metabolic adaptation plateaus
5 Common Myths
Eating carbohydrates must be minimized in order to make blood sugars easier to control in the long term.
Complex carbohydrates such as whole grains and legumes are necessary to provide slow energy and glucose level regulation due to fiber slowing the absorption of these foods. Research shows diets containing 45-60% carbohydrates, particularly from unrefined and unprocessed sources improve insulin sensitivity and reduce HbA1c more than extreme low carbohydrate diets. The timing of these carbohydrates can also be useful in optimizing glucose utilization by the body especially when physical activity is taken into account, thus making the elimination of carbohydrates unnecessary.
Once you initiate insulin therapy, you never stop it.
Many type 2 diabetics can come off insulin positively by making modifications in lifestyle which are capable of restoring natural glucose control. Insulin through reduction of weight in a targeted way, development of muscle through exercise and reduction of stress enhances the functional reserve of pancreatic beta-cell function to the extent that glucose can be effectively controlled without insulin. Continuous glucose monitoring will often show that insulin is no more necessary after sustained correction in insulin sensitivity and recovery of pancreatic beta-cell function.
People with diabetes should avoid all fruits because they're sugary.
Whole fruits like berries, apples, and citrus have low glycemic impact due to their fiber matrix and polyphenol content slowing sugar absorption. Studies demonstrate daily fruit consumption actually lowers diabetes risk by 7-13% because fruits' antioxidants improve insulin signaling. Portion-controlled fruits paired with protein or fats provide vital nutrients without significant glucose spikes when consumed strategically.
All artificial sweeteners are safer than sugar with regards to glucose control.
Certain artificial sweeteners disrupt gut microbiota and insulin response in ways that paradoxically impair glucose tolerance over time. Studies link chronic consumption of sucralose and saccharin with decreased insulin sensitivity and increased fasting blood glucose. Natural alternatives like monk fruit or stevia show better metabolic safety profiles without inducing sweet taste receptor confusion that promotes glucose spike.
It is inevitable that between-meal snacking will raise your blood sugar.
Intelligently chosen snacks that are balanced in macronutrients will stabilize glucose, giving you less extreme hunger which leads to overeating. Foods like nuts, cheese or vegetables for snacks containing protein or fiber taken 3-4 hours after meals will maintain insulin sensitivity without raising glucose levels markedly. Monitoring glucose with continuous glucose monitors shows that properly time snacks are able to lessen glucose variability by 27 % as compared with large, infrequent meals.
Conclusion
Gaining command of blood sugar means seeing the natural rhythms and responses of your body. There is a teamwork of hormones in the interplay of insulin and glucagon that assures balance when given the proper support. The direct choices we make each day can either enhance or disrupt these built-in mechanisms. Your unique biology ensures that you require personal endeavors to achieve what is best for you.
Expert guidance helps you customize recommendations for your unique metabolic patterns. What works to stabilize blood glucose for one may be the opposite for another individual. Continuous assessment shows your own responses and thresholds. This individualized monitoring avoids the pitfalls that result from general advice and misses the mark.
Sustainable habits always topple quick fixes. Small, consistent changes, such as regular movement and balanced meals, yield compounding returns. Sharp limits often backfire, creating an infeasible cycle. Long-term stability comes from routines that naturally fit your lifestyle.
These principles create the metabolic resiliency that develops further through the years. Continued support for the body's systems prevents future complications from arising. You make permanent health through your cooperation with your physiology. This knowledge changes the management of glucose from a burden to empowered self-care.
External Sources
Frequently Asked Questions
How does the body naturally regulate blood sugar?
The pancreas maintains blood sugar balance through insulin and glucagon hormones. Insulin lowers glucose by storing it in cells after eating, while glucagon raises glucose during fasting by releasing stored energy. This hormonal interplay keeps levels within a healthy range.
What lifestyle factors most impact blood sugar stability?
Key lifestyle elements influencing glucose control include:
- Consistent sleep patterns regulating cortisol and insulin sensitivity
- Regular physical activity increasing glucose uptake into muscles
- Balanced meal timing preventing extreme highs and lows
- Stress reduction techniques minimizing cortisol-triggered glucose release
- Hydration maintaining optimal kidney function for glucose processing
Which foods best support healthy blood sugar levels?
Optimal foods combine fiber, protein, and healthy fats:
- High-fiber whole grains slowing carbohydrate absorption rates
- Lean proteins like poultry and fish improving insulin response
- Healthy fats from avocados and nuts reducing meal spikes
- Low-glycemic fruits such as berries providing antioxidants
- Vinegar-containing foods enhancing insulin sensitivity naturally
How does sleep quality affect blood sugar regulation?
During deep sleep stages, the body optimizes insulin sensitivity and repairs glucose metabolism pathways. Poor sleep disrupts cortisol rhythms and growth hormone release, leading to insulin resistance. Consistent 7-9 hour sleep maintains hormonal balance for stable morning glucose levels.
What exercise strategies best stabilize glucose?
Effective approaches include:
- Pre-meal walking activating glucose transporters before eating
- Resistance training building muscle mass for better storage
- Post-meal movement utilizing circulating blood glucose
- Consistent daily activity patterns enhancing insulin sensitivity
- High-intensity intervals boosting metabolic rate long-term
What are warning signs of unstable blood sugar?
Common indicators include:
- Persistent fatigue and energy crashes between meals
- Increased thirst and frequent urination patterns
- Difficulty concentrating or brain fog episodes
- Unexplained weight changes without diet modifications
- Slow healing of minor cuts or skin infections
How does stress influence blood glucose levels?
Stress triggers cortisol release which signals the liver to produce extra glucose for fight-or-flight responses. Chronic stress creates sustained high glucose and insulin resistance. Managing stress through breathing techniques and mindfulness prevents these physiological disruptions.
Can specific foods dangerously spike blood sugar?
The most disruptive foods include:
- Refined carbohydrates without fiber or protein buffers
- Sugar-sweetened beverages causing rapid glucose surges
- Highly processed snacks with hidden added sugars
- Fried foods combining carbs with inflammatory fats
- Large fruit portions consumed without protein pairing
What hydration practices support glucose control?
Optimal hydration involves:
- Drinking water before meals to moderate appetite
- Including electrolytes during prolonged activity periods
- Choosing herbal teas over sugary beverages
- Monitoring urine color for hydration adequacy
- Limiting fluids during meals to avoid enzyme dilution
How does meal sequencing affect blood sugar?
Eating order significantly impacts glucose absorption:
- Starting meals with vegetables and proteins first
- Adding healthy fats before complex carbohydrates
- Including vinegar or lemon juice with meals
- Allowing 3-4 hours between eating sessions
- Avoiding late-night snacks before sleep